Byram W. Bridle, University of Guelph; Samira Mubareka, University of Toronto, and Shayan Sharif, University of Guelph
Athletes understand that there are two very different approaches that can be taken when training their bodies. For example, lifting heavy weights is a great way to achieve maximum strength. In contrast, low-load high-repetition training is ideal for developing the stamina required for endurance sports.
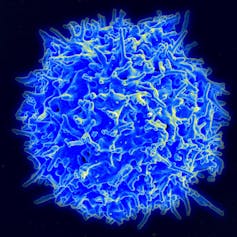
Remarkably, our immune system can be trained in a somewhat similar fashion. It must choose between two different responses to dangerous pathogens, both of which lead to white blood cells called T cells and antibodies targeting the infecting microbe.
However, the types of these T cells and antibodies is different depending on whether the pathogen lives outside of our cells, as many bacteria do, or inside our cells, as viruses do.
Mounting an anti-bacterial response against a virus may not be an ideal way to clear a viral infection. In fact, the wrong kind of immune response can actually exacerbate disease, as was observed in vaccinated mice challenged with the severe acute respiratory syndrome coronavirus (SARS-CoV) identified in 2003.
Importantly, our first exposure to a pathogen, either naturally or via vaccination, can train our immune system to adopt one of these two biases when we respond in the future to the same or a similar pathogen for the rest of our lives. Immunologists call this “trained immunity.”
First exposure
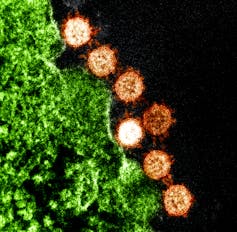
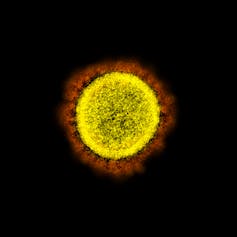
Our research programs span the fields of viral transmission, immune responses to viruses, respiratory pathogens such as influenza viruses and vaccine development, including vaccines against SARS-CoV-2, which is the causative agent of the coronavirus disease that emerged in 2019, COVID-19.
We would like to convey the importance of trained immunity in the context of COVID-19 vaccines since this can have implications for the ability of our immune systems to respond appropriately to highly pathogenic coronaviruses in the future.
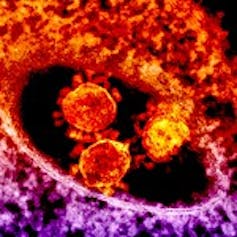
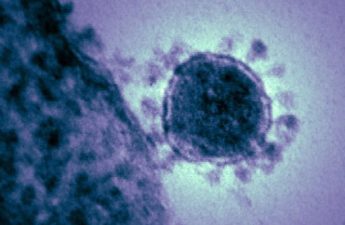
Over the past 17 years, there have been three major outbreaks of highly pathogenic coronaviruses: the original SARS-CoV in 2003, Middle East Respiratory Syndrome coronavirus in 2012 and now SARS-CoV-2.
Based on this history of having a new highly pathogenic coronavirus emerge approximately every decade, we should expect to have to deal with more of these viruses in the future. That means that the current drive to develop vaccines for COVID-19 should consider future coronavirus outbreaks.
The way we train our immune systems now to respond to SARS-CoV-2 could impact how well our bodies can respond to future coronaviruses. Vaccines, if developed properly, provide an opportunity to induce the type of trained immunity that is optimal for mounting protective immune responses, not only against SARS-CoV-2, but also against future infections with coronaviruses and/or their associated vaccines.
Tuberculosis response
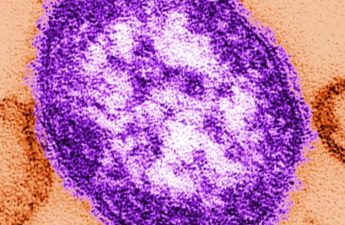
Interestingly, some scientists have proposed to harness the concept of trained immunity in a related context. Specifically, there is evidence to suggest that individuals who received a vaccine against tuberculosis may be partially protected against SARS-CoV-2.

Tuberculosis is a respiratory disease caused by a bacterium. In contrast to many bacteria, this one, like viruses, lives inside cells. The vaccine formulation uses a live, but attenuated (modified or weakened) bacterium that is very similar to the one that causes the disease. Since it is a live bacterium, it can infect cells in the same way that the disease-causing bacteria do.
The result is an appropriate immune response that happens to be of the same type that is optimal against viruses. Scientists have concluded, therefore, that the tuberculosis vaccine might be training the immune system in such a way that it can respond ideally to other pathogens that live inside cells, including viruses like SARS-CoV-2.
Evaluating responses
A heavy emphasis is being placed on quantitative aspects of candidate COVID-19 vaccines, such as whether they generate high levels of antibodies. Many health regulatory agencies are poised to approve COVID-19 vaccines that reduce the burden of disease but do not induce immunity to completely prevent infection and transmission. But they should be cautious and ensure that these vaccines do not train our immune system for a response that is not optimal.
By thoroughly evaluating the nature and duration of the immune response induced by a prospective COVID-19 vaccine, we can ensure specific, effective and sustained responses against SARS-CoV-2. Specifically, vaccine developers should be able to answer these questions:
- Did the vaccine induce an immune response that is optimal against viruses? A balanced antiviral response should include antibodies to prevent the virus from infecting host cells and replicating inside them, and T cells to kill viruses that get past the antibody barrier. Importantly, the antibodies should be of antiviral types.
- Were there antibody responses in the respiratory tract, and do these antibodies efficiently neutralize the virus? There is significant focus placed on measuring antibody responses in the blood, but SARS-CoV-2 infects mucosal surfaces including the respiratory tract, and it is important to ensure that the vaccine induces antibodies at these relevant locations. Also, it must be noted that appropriate antibody responses against viruses are usually of much lower magnitude than those directed against extracellular bacteria. A large quantity of antibodies may seem promising, but the amount is not nearly as important as the types and locations of these antibodies.
The take-home message is that we should insist on maintaining a very high standard for a COVID-19 vaccine; one that will induce a qualitatively appropriate immune response that will protect us from infection with SARS-CoV-2.
Like an athlete, we need to avoid training our immune system in a way that contradicts the end goal. For long-term health, we must ensure that our immune systems are trained in a way that will allow us to respond most effectively against future highly pathogenic coronaviruses, some of which may prove to be more dangerous than the current one.
Byram W. Bridle, Associate Professor of Viral Immunology, Department of Pathobiology, University of Guelph; Samira Mubareka, Clinician-scientist, Laboratory Medicine and Pathobiology, University of Toronto, and Shayan Sharif, Professor of Immunology and Associate Dean, Research and Graduate Studies, University of Guelph
This article is republished from The Conversation under a Creative Commons license. Read the original article.