Facilities that convert to Rural Emergency Hospital status will get a 5% increase in Medicare payments as well as an average annual facility fee payment of about $3.2 million in exchange for giving up their expensive inpatient beds and focusing solely on emergency and outpatient care. Rural hospitals with no more than 50 beds that closed after the law passed on Dec. 27, 2020, are eligible to apply for the new payment model if they reopen.
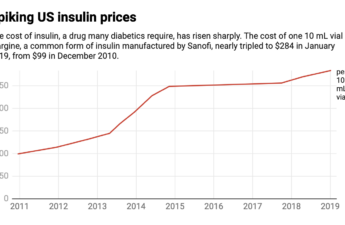
Eli Lilly is cutting insulin prices and capping copays at $35 – 5 questions answered
High insulin prices have not earned any U.S. manufacturer many friends, with list prices increasing 54% from 2014 to 2019. Most troublingly, an estimated 1.3 million uninsured people with diabetes and patients with inadequate insurance have resorted to rationing their insulin. Skipping doses because of high insulin prices has sometimes had tragic and even deadly consequences.But growing competition has shaken up the insulin market in recent years.
Where are we at in King County with COVID-19?
A conversation with Seattle King County-Public Health’s Dr. Jeff Duchin, the county’s health officier and chief of Communicable Disease Epidemiology & Immunization Section.
Masking requirements in healthcare, long-term care, and correctional facilities to end April 3 in Washington state.
DOH infection prevention and control guidance continues to recommend masks for patients, healthcare providers, and visitors in healthcare settings. Licensed healthcare facilities are required to have infection prevention policies and programs consistent with CDC guidance.
Exercise is even more effective than counselling or medication for depression. But how much do you need?
We found the higher the intensity of exercise, the more beneficial it is. For example, walking at a brisk pace, instead of walking at usual pace. And exercising for six to 12 weeks has the greatest benefits, rather than shorter periods. Longer-term exercise is important for maintaining mental health improvements. When comparing the size of the benefits of exercise to other common treatments for mental health conditions from previous systematic reviews, our findings suggest exercise is around 1.5 times more effective than either medication or cognitive behaviour therapy.
Beware of Fraudulent Coronavirus Tests, Vaccines and Treatments—FDA warns
The FDA is particularly concerned that these deceptive and misleading products might cause people to delay, skip or stop appropriate medical treatment for COVID-19, leading to serious and life-threatening harm. It’s likely that the products do not do what they claim, and the ingredients in them could cause adverse effects (bad reactions) and could interact and potentially interfere with medications to treat many underlying medical conditions.
Surprise-Billing Law Loophole: When ‘Out of Network’ Doesn’t Quite Mean Out of Network
Referred to Swedish Maternal & Fetal Specialty Center – First Hill for pregnancy complications, Danielle Laskey, a registered nurse, was surprised with a $120,000 hospital bill.
80% of pregnancy-related deaths in Washington state were preventable, study
Behavioral health conditions, including suicide and overdose, remain the leading causes of pregnancy-related deaths. Other common causes were hemorrhage and infection.
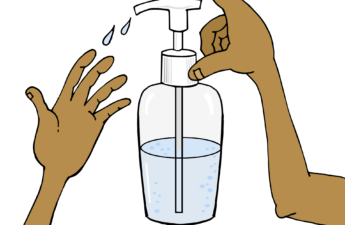
One easy way to fight antibiotic resistance? Good hand hygiene
Hygiene and antibiotic use interact. Antibiotic use had less of an effect on the evolution of antibacterial resistance as hygiene levels increased. This is because evolution toward resistance depends on variation in bacterial sensitivity to antibiotics. By affecting the distribution of resistant and sensitive bacterial strains across patients, hygiene limits the bacterial diversity needed to evolve resistance.
Considering going off antidepressants? Here’s what to think about first
Stopping antidepressants abruptly, especially after a long period of use, will make most people – although not everyone – unwell. It’s impossible to tell in advance who will be affected, so slow dose reduction is advisable. Stopping antidepressants (or tapering down the dose) too rapidly can cause antidepressant discontinuation syndrome in around 20% of people.
What is delirium?
Up to one-third of older people admitted to hospital are diagnosed with delirium. This increases the risk of unnecessary functional decline, a longer hospital stay, falls, needing to be admitted to a residential aged care facility, and death. However, identifying the condition early reduces these risks. Delirium can also be prevented by identifying who is vulnerable to the condition and finding ways of reducing the person’s risk.
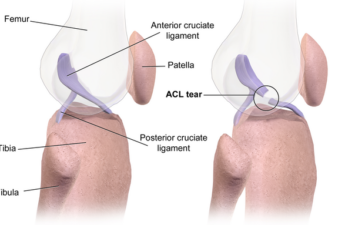
Female football players are at much higher risk of career-ending ACL injuries – the science on why
Females have a wider pelvis relative to leg length, which results in increased angulation at the knee. The shape of the bones is also different in women in that the ACL passes through a narrower space to attach to the thigh bone, which may make it more susceptible to injury. The actual size of the ACL is also often smaller in females, so may be less able to withstand high forces.
Rejecting science has a long history – the pandemic showed what happens when you ignore this
Anti-vaccination groups, as well as other anti-science movements, are not new phenomena, nor are the nature of their objections. Most anti-science arguments have been around for centuries.
Addiction Treatment May Be Coming to a Pharmacy Near You
new study showed patients who receive the medicine at pharmacies rather than at doctor’s offices stayed in treatment longer.
The fungus zombies in ‘The Last of Us’ are fictional, but real fungi can infect people, and they’re becoming more resistant
Many of the people watching The Last of Us are likely there for the zombies. I love the zombies too, but I’m really there for the fungus.